What is Clinical Biochemistry
Clinical Biochemistry involves the use of biochemical measurements to support the diagnosis, treatment, prevention and monitoring of disease. Measurements are made in blood, urine, cerebrospinal fluid and other body fluids.
Biochemical measurements can assist in determining the
function of the kidneys, liver, heart, thyroid and other endocrine organs as well as assessing cardiovascular risk by measuring lipids (including cholesterol), or diagnosing and monitoring diabetes.
Increasingly, Clinical Biochemistry tests are also used as a means of determining which patients would benefit from and, just as importantly would not, more invasive procedures and/or expensive therapies.
Clinical Biochemistry Departments
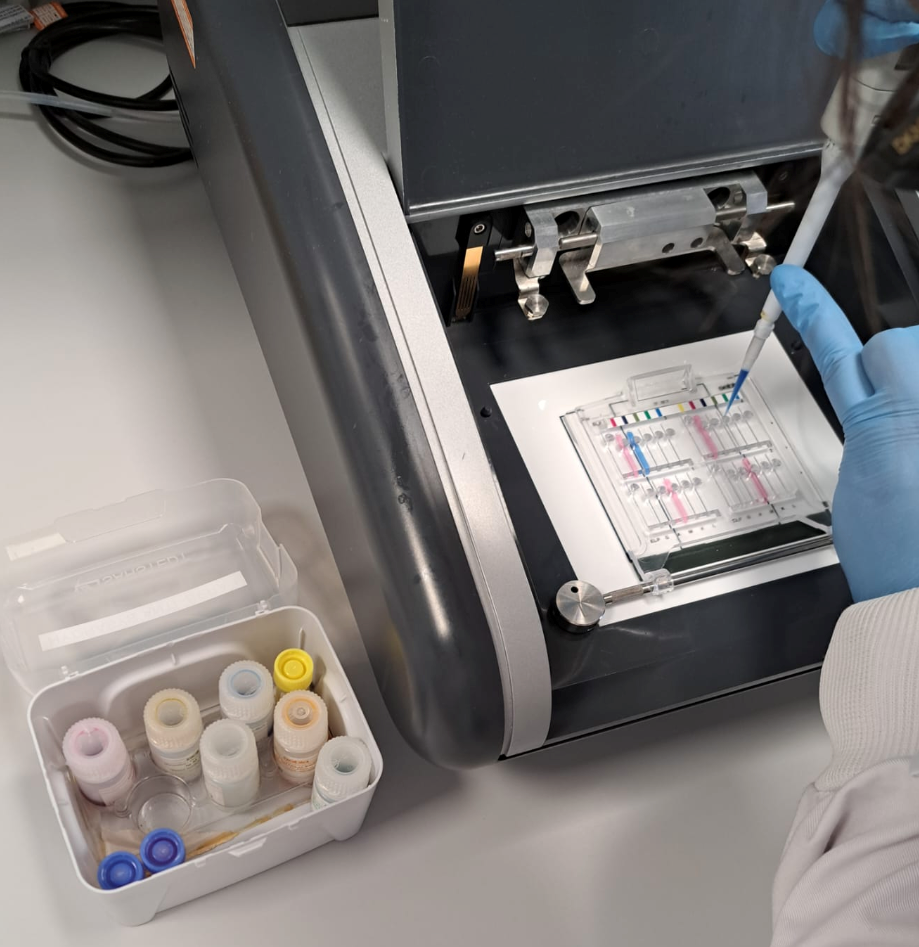
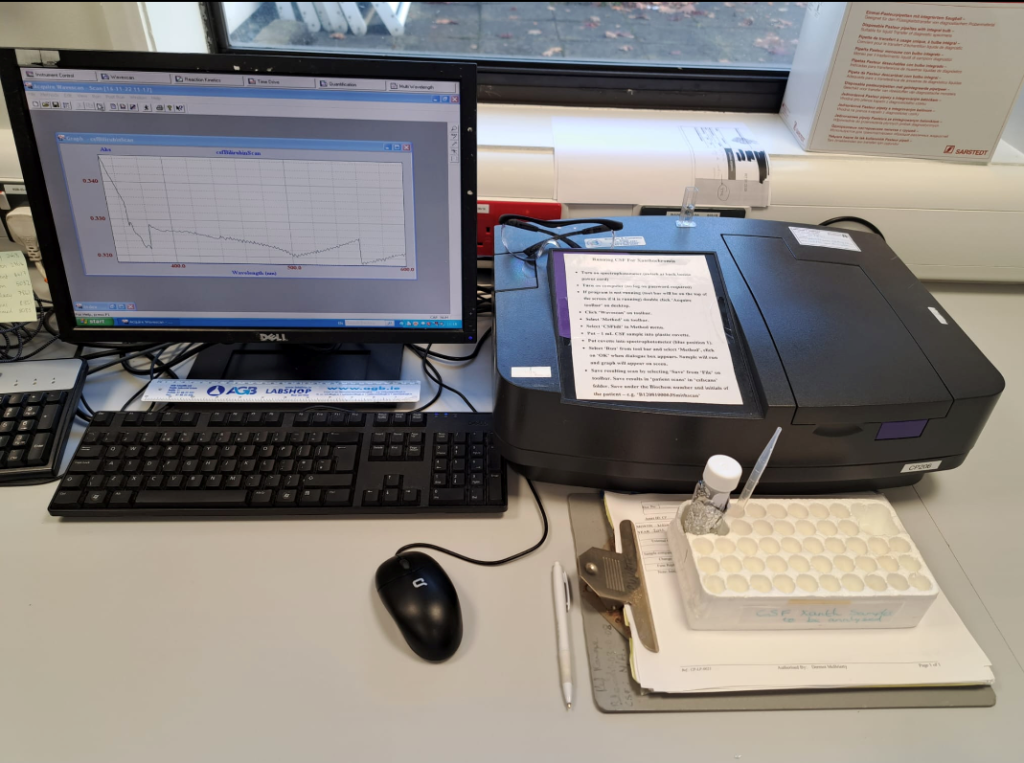
Clinical Biochemistry departments usually operate within a hospital and are responsible for providing biochemical testing to the highest standards. They typically provide a service for in-patients and out-patients as well primary care. Such departments make extensive use of information technology and robotics. Tests required in large numbers (such as potassium and urea in blood) are analysed on highly sophisticated automated equipment. Other techniques used in Clinical Biochemistry laboratories may include immunoassay, electrophoresis, many types of chromatography, mass spectrometry, and DNA technology. Most clinical biochemistry laboratories are accredited to ISO 15189 standards.
Near patient testing, or point of care testing is carried out in the patient’s location rather than in the laboratory. Biochemistry is one of the core near patient testing disciplines, supporting the use of glucose and blood gas testing close to the patient, among other analyses.
Most departments will carry out research and develop and investigate new and improved analytical methods. A number of sub specialities exist within the general area of Clinical Biochemistry including Paediatrics, Endocrinology, Biochemical genetics, Toxicology, and Molecular Biology.
The role of the Clinical Biochemist
The post of biochemist has a long standing place in the Irish healthcare system, commencing in the late 1940’s and early 1950s. The Fitzgerald report (1968) identified a deficiency of scientific knowledge within the hospital pathology diagnostic services and recommended the urgent establishment of a new career structure for hospital biochemists.
Since that time the role of Clinical Biochemists has evolved in their contribution to the delivery of clinical biochemistry and diagnostic endocrinology services throughout Ireland.
In broad terms the contribution of the biochemist may be defined through clinical, scientific, quality, management and leadership roles. For the latter, more senior members of the profession are Heads of Department and are responsible for the clinical and scientific governance and strategic direction of clinical biochemistry services in Ireland.
All roles and responsibilities which define a clinical biochemist’s scope of practice are commensurate to their training, development and experience.
Clinical Biochemists play key roles in service development by applying their scientific knowledge, skills and expertise. Through horizon scanning and clinical liaison Clinical Biochemists develop clinical biochemistry services with a view to meeting clinical need, currently and in the future. They introduce and develop the latest diagnostic tests to ensure optimal patient diagnosis and management. In this regard, Clinical Biochemists have developed significant expertise nationally and have embraced important technologies such as Mass Spectrometry and Next Generation Sequencing. Clinical Biochemists drive translational research, introduce new developments into service and publish such work in clinical and scientific manuscripts in peer-reviewed science and medical journals. Such work is also presented at local meetings, and at national and international conferences (poster or oral presentations).
Clinical Biochemists undertake many clinical duties commensurate with their training which include clinical interpretation and advice to all clinical users of the service. This includes advice and guidance on appropriate further testing to support GPs in diagnosis and appropriate management as well as supporting hospital-based teams for diagnosing and monitoring more complex patients. This advice is often delivered in writing, through result reports and letters as well as verbally through telephone conversations, participation at Multi-Disciplinary Team (MDT) meetings and case discussions.
Clinical Biochemists are responsible for ensuring the quality of clinical biochemistry and diagnostic endocrinological investigations, fulfilling not only the requirements for laboratory accreditation (ISO 15189), but initiating and leading other quality improvements which further help to mitigate risk and ultimately help maintain patient safety. Clinical Biochemists are involved in the verification and validation of new assays, ensuring that they meet the relevant analytical, clinical and quality standards. Clinical Biochemists play key advisory roles in External Quality Assurance/Assessment programmes both nationally (e.g. Irish External Quality Assurance Scheme) and in the UK (UK National External Quality Assessment Services). Clinical Biochemists also undertake accreditation inspection roles, working with the Irish National Accreditation Board (INAB) and the UK National Accreditation Scheme (UKAS).
Clinical Biochemists have key roles in national and international clinical and scientific bodies and initiatives where they are involved in providing professional and expert advice in the development of best practice guidance and policies. Beyond those mentioned already, these include the National Cancer Control Programme (NCCP), the National Gestational Trophoblastic Disease Registry, the Irish Endocrine Society (IES), the Faculty of Pathology (RCPI), the Health Information and Quality Authority (HIQA), the National Office of Clinical Audit (NOCA) and the Royal College of Pathologists
(UK).
As the national society for the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM), and the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC), the ACBI’s clinical biochemist members contribute to many EFLM and IFCC task forces, working groups, publications and educational material.
Clinical Biochemists play an important role in teaching activities within hospitals and universities, to undergraduate and postgraduate (MSc, PhD) science and medical students. More senior Clinical Biochemists are also involved in the scientific and clinical training of Clinical Biochemists in the earlier stages of their careers, including those Clinical Biochemists who undertake clinical training with Fellowship examinations through the Royal College of Pathologists (FRCPath, UK). Clinical Biochemists are also involved in the training of other professions working in laboratory medicine
including Medical Scientists and Pathologists.
Clinical Biochemists provide educational input outside the laboratory by presenting at hospital grand rounds, journal clubs, GP Liaison forums and educational meetings of other health and social care professionals.